Peripheral Neuropathy involves damage to the nervous system. There are two parts to the nervous system, central and peripheral. The central nervous system includes the brain and spinal cord, while the peripheral nervous system includes all the nerve roots that come off of the spinal cord (and then the nerves they turn into).
These nerve roots turn into extremity nerves (peripheral nerves) such as the sciatic nerve,  median nerve and ulnar nerve that transmit motor and sensory information to the arms and legs. These nerves perform functions such as flexing your arm, telling your arm to feel hot or cold, or experiencing pain. With a peripheral neuropathy, some of these transmissions may be altered.
median nerve and ulnar nerve that transmit motor and sensory information to the arms and legs. These nerves perform functions such as flexing your arm, telling your arm to feel hot or cold, or experiencing pain. With a peripheral neuropathy, some of these transmissions may be altered.
The symptoms of a peripheral neuropathy may include numbness, tingling, pins and needles sensation or muscle weakness. When severe, symptoms may include muscle wasting, paralysis, burning pain, or gland dysfunction. Eventually, neuropathy may reach a point where there’s no more pain, because there is no more sensation.
There are three different types of peripheral neuropathy:
- Mononeuropathy – one nerve is damaged
- Polyneuropathy – several nerves with multiple limbs affected
- Mononeuritis multiplex – two or more nerves in different areas of the body
Diabetic neuropathy is the most common form of peripheral neuropathy. It is a polyneuropathy. Usually it affects one’s feet, then travels up both legs. It can also affect the fingers and hands moving up a person’s arms. It does not affect individuals equally.
Mononeuropathy is a situation that affects one nerve, such as carpal tunnel syndrome. In the case of carpal tunnel, the median nerve is compressed. This may cause severe pain and muscle weakness, or might just be a nuisance from time to time.
The mononeuritis multiplex situation is a painful condition that involves at least two separate nerves. This may be associated with Lyme disease, amyloidosis, rheumatoid arthritis and more. It is the least common of the peripheral neuropathy varieties.
HOW IS PERIPHERAL NEUROPATHY CAUSED?
The most common reason one develops preipheral neuropathy is from uncontrolled diabetes. With diabetes affecting over 16 million Americans, the potential for ending up with diabetic neuropathy, which is the most common subset of peripheral polyneuropathy, is fairly high. According to the World Health Organization, by the year 2025 one third of Americans will have diabetes. That is a large number!
Call (602) 507 – 6550 to schedule your Appointment TODAY!
Here’s a list of some other reasons that individuals develop peripheral neuropathy:
- Heavy alcohol intake over a long period of time
- Diet issues and malnutrition such as low vitamin B12 levels
- Thyroid under-activity
- Insufficient blood flow to one’s legs
- Chronic kidney problems
- Systemic lupus or rheumatoid arthritis
- Liver infections or HIV
- Drugs or radiation effects from the treatment of cancer, seizures or infections
- Heavy-metal toxicity such as with mercury or lead.
WHAT ARE PATIENTS SYMPTOMS FROM PERIPHERAL NEUROPATHY?
Symptoms between patients will vary, with the feet usually being affected first. Early neuropathic signs may include tingling or burning in the feet which can begin to travel up a person’s legs.
Unlike sciatica, peripheral neuropathy symptoms usually involve both lower extremities.

That is, unless a person has a mononeuropathy such as a tarsal tunnel syndrome. In this case, usually it involves just one extremity.
With a progressive neuropathy, usually sensation starts to be lost in the feet and can make walking difficult since people do not feel their feet properly under their body.
As sensation is lost, patients may start to develop sores or ulcers, along with an inability to differentiate cold from hot temperatures on their feet. As sensation is lost, the burning pain that is often associated with peripheral neuropathy may turn more into a dull ache and then eventually with severity sensation may go away altogether.
Unfortunately, peripheral neuropathy may also lead to weakness of muscles which may cause people difficulty with walking, making a cane or walker necessary. If the neuropathy involves the hands and arms as well, it may be tough for people to perform hygiene activities along with buttoning shirts or hand writing.
Outside of the neurologic symptoms, organ dysfunction may occur along with erectile dysfunction, bladder leaking, digestive issues or cardiac problems.
How is peripheral neuropathy worked up by doctors?
A careful history and physical exam will help along with a set of blood work to look for common electrolyte abnormalities and evidence of inflammatory disorders like rheumatoid arthritis.

Imaging studies such as x-rays or MRI can show the extent of arthritis or joint destruction along with evidence of nerve compression. In the case of a disc herniation or a peripheral nerve being pinched such as with tarsal tunnel syndrome, an MRI can show the extent of compression.
Additional studies that may be helpful include an electromyography or a nerve conduction velocity study, this is commonly known as an EMG or NCV. The doctor my also order a gate study analysis and possibly a muscle biopsy to look for additional issues.
What kind of treatments are available to suppress the symptoms and also make the neuropathy better?
Medications
There are multiple medications available to help moderate the symptoms of peripheral neuropathy. Pain medications that are either narcotic or non-narcotic (e.g Tramadol) can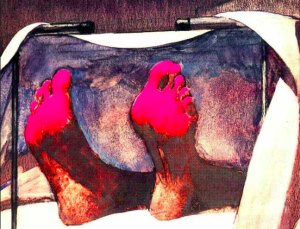 provide substantial relief. It is not the best idea to use these on a long-term basis as there are substantial risks associated with chronic narcotic usage.
provide substantial relief. It is not the best idea to use these on a long-term basis as there are substantial risks associated with chronic narcotic usage.
Neurologic modifying medications such as Neurontin or Lyrica can help to modulate and decrease the burning symptoms from neuropathy. We actually do not know exactly how these medications work, but they can be very effective.
Mild to moderate pain can often be helped with over-the-counter medications such as anti-inflammatories and Tylenol. There are various antidepressant medications that can help modulate the pain from neuropathy. These are used in an off-label fashion, since they were actually developed for depression.
Call (602) 507 – 6550 to schedule your Appointment TODAY!

Physical Therapy and Chiropractic
Physical therapy and chiropractic treatment may help modulate the symptoms somewhat from neuropathy. They do not alter the nerve problems that occur with painful neuropathy, but that may help to increase blood flow to the area and reduce pain.
Massage may help with symptoms along with ultrasound, electrical stimulation or a TENS Unit.
Pain Management Procedures
Interventional procedures for helping with neuropathy pain include injections of numbing medicine and steroid depending on whether or not there is one nerve rbeing compressed or many. In the case of a mononeuropathy from carpal tunnel syndrome, tarsal tunnel syndrome or a disc herniation with compression and sciatica, these injections can be very 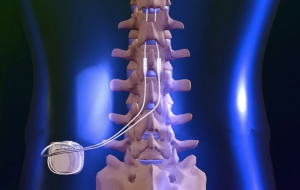 Pain Specialists is the best pain management practice in the Phoenix and Scottdsale metropolitan area.
Pain Specialists is the best pain management practice in the Phoenix and Scottdsale metropolitan area.
Arizona Pain has Board Certified and Award Winning AZ pain doctors and chiropractors who can help alleviate the pain from neuropathy and work in conjunction with your primary doctor to help get to the root cause of the problem. If this includes poorly controlled diabetes, getting the blood sugars under control can help stop the progressive nature of the diabetic neuropathy.
Call (602) 507 – 6550 to schedule your Appointment TODAY!

![]()

 median nerve and ulnar nerve that transmit motor and sensory information to the arms and legs. These nerves perform functions such as flexing your arm, telling your arm to feel hot or cold, or experiencing pain. With a peripheral neuropathy, some of these transmissions may be altered.
median nerve and ulnar nerve that transmit motor and sensory information to the arms and legs. These nerves perform functions such as flexing your arm, telling your arm to feel hot or cold, or experiencing pain. With a peripheral neuropathy, some of these transmissions may be altered.


 provide substantial relief. It is not the best idea to use these on a long-term basis as there are substantial risks associated with chronic narcotic usage.
provide substantial relief. It is not the best idea to use these on a long-term basis as there are substantial risks associated with chronic narcotic usage.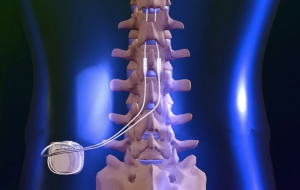 Pain Specialists is the best pain management practice in the Phoenix and Scottdsale metropolitan area.
Pain Specialists is the best pain management practice in the Phoenix and Scottdsale metropolitan area.